The fight against the HIV/AIDS pandemic has myriad weapons at its disposal, such as educational tools; cheap and effective diagnostics; and antiviral drugs used to suppress virus replication, stop disease and onward transmission, but one thing that has proven to be very difficult is curing all the people infected who are unable to eliminate the virus. The difficulty here is that HIV is an expert at hiding from us while inside our own body. Although premature, recent news reports from ongoing trials in the UK have led to talk of an HIV cure using an experimental approach to rid our bodies’ of the virus, but what is the science behind these approaches? And why are we bothering with them anyway?
Two of the major goals of HIV research are to develop a vaccine to prevent new infections, and develop a way to cure all the millions of people currently infected. Yet both goals have not been reached. According to the World Health Organisation (WHO), 36.7 million people are infected currently with HIV-1 (the most common type of the virus in man) and only less than half of those infected are being treated with antiviral drugs. Unfortunately, the number of new people infected each year is not dropping as dramatically as we would like, suggesting that we are not yet winning the war against this pandemic on a global level.
Shock and kill
Curing somebody from an HIV infection is challenging because of the fundamental biology of the virus (see this for an excellent free review of this). HIV is a retrovirus, which means that it replicates by inserting a DNA copy of its entire genome (which is composed of RNA) into the genome of the cell that has just been infected. From this DNA copy new RNA genomes are made. Once that copy is there then it cannot be removed. Although, one of the only ways that the DNA copy could be removed from our body naturally would be through the death of that infected cell yet that might not be as straightforward as it might seem.
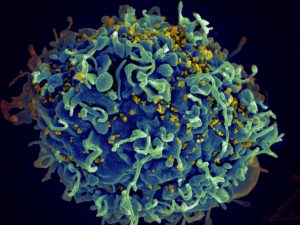
HIV can infect a kind of immune cell (specifically a T cell) that has the ‘CD4’ glycoprotein on its surface (CD4+ve ‘helper’ T cells). These cells from a part of our natural immune response where they interact with other immune cells and can promote an effective response. T cells are a part of the adaptive ‘memory’ immune system and as a consequence can live for a very long time. As HIV infects these cells, the inserted DNA copy also survives for years, still capable of producing new viruses. The long-lived ‘resting’ cells however, don’t produce a lot of HIV, yet during some conditions these cells can become ‘activated’, causing them to divide, inducing the production of new HIV genomes, viruses and sustaining the infection.
HIV antivirals stop these genomes producing infectious viruses and infecting new cells but cannot touch the DNA copy residing in long-lived cells. A complete cure would have to eliminate any traces of HIV DNA from our cells that has the capacity to produce new viruses. One strategy would be to activate HIV genome production at once in combination with a way to kill or block new infections, which is known as ‘shock and kill’.
Shock and kill has a long history with many attempts focusing on using antivirals, neutralising antibodies or by promoting our own immune cells to kill the newly activated cells. This approach is challenging because of the need to balance viral activation without producing lots of activated and readily-infectable T cells and effective combination with an additional therapeutic, such as antivirals or antibodies that only block onward infection. Another example, the RIVERS trial used a histone deacetlyase (HDAC) inhibitor (cellular HDACs prevent HIV genome production – their inhibition forces HIV production) along with an anti-HIV vaccine regime (chimpanzee adenovirus followed by modified vaccinia Ankara (MVA) virus boost). However, this is an area of active research and a recent paper suggests that we could achieve HIV activation, kill those activated cells and block onward infection using a single drug, just by exploiting our own bodies’ natural antiviral response.
Innate immunity to the rescue
Li et al., reporting in Nature Medicine earlier in the summer, show that by administration of a drug Acitretin – a derivative of retinoic acid, which is itself a metabolite of vitamin A – to human cells in the lab infected with HIV, they can kill cells that are infected with HIV.
The secret to how this is achieved is via the simultaneous induction of HIV RNA production and a human gene called DDX58, otherwise known as ‘retinoic acid-inducible protein-I’ (RIG-I) (which is known to be induced by retinoic acid and its derivatives).
RIG-I is a very important antiviral protein that can detect viral RNA within the cytoplasm of a cell and kick-start an antiviral response, which can be characterised by cell death (apoptosis) and secretion of antiviral signalling proteins called interferons. In the case of Li et al., their anti-HIV affect following Acitretin treatment was dependent on RIG-I and associated with apoptosis and interferon production; apoptosis would destroy infected cells and the interferon may protect nearby cells through the production of interferon-stimulated gene products (and help induce apoptosis) that are not infected yet, thus preventing the spread of infection.
Notably, this strategy differs from the RIVERS approach in that it exploits our innate immune system, rather than our adaptive.
Is this a cure?
The simple answer is no. Or at least, not yet. While this study is a nice idea, with potential, the work was carried out only in cells in the lab (although it included primary cells from patients with HIV). There are concerns whether these cells isolated from the bloodstream are representative of the long-lived T cells (and other kinds of cells) infected with HIV found deep in the organs of patients. Other problems could appear when translating this work into animal models and the clinic: would systemic treatment with Acitretin would reach all the infected cells? And how would your body react if all cells reactivated their infection, inducing apoptosis and interferon production, simultaneously? Might there be unwanted side-effects related to reactivation? Or even from Acitretin itself?
While a cure using this Li et al’s, shock and kill approach is a long way off, any cure would be an incredible tool in our response to the HIV pandemic and it is fascinating to see such diverse preclinical experimental options. The same issues that would stem from taking this RIG-I approach through the clinic are the same ones that studies like the RIVER study have met. We look forward to seeing the results from the RIVERS trial and how other ‘shock and kill’ studies perform in the future.
By Connor Bamford, Ph.D (@cggbamford)
****************************************************
CVR investigators carry out comprehensive research on HIV and related retroviruses, looking at HIV evolution in patients, animal retroviruses, cancer-causing retroviruses and how our innate immune system defends ourselves against them. These labs include, the Neil, Gifford, Hosie, Thomson, Willett and Wilson labs.

